Predictive Analytics in Medical Diagnosis
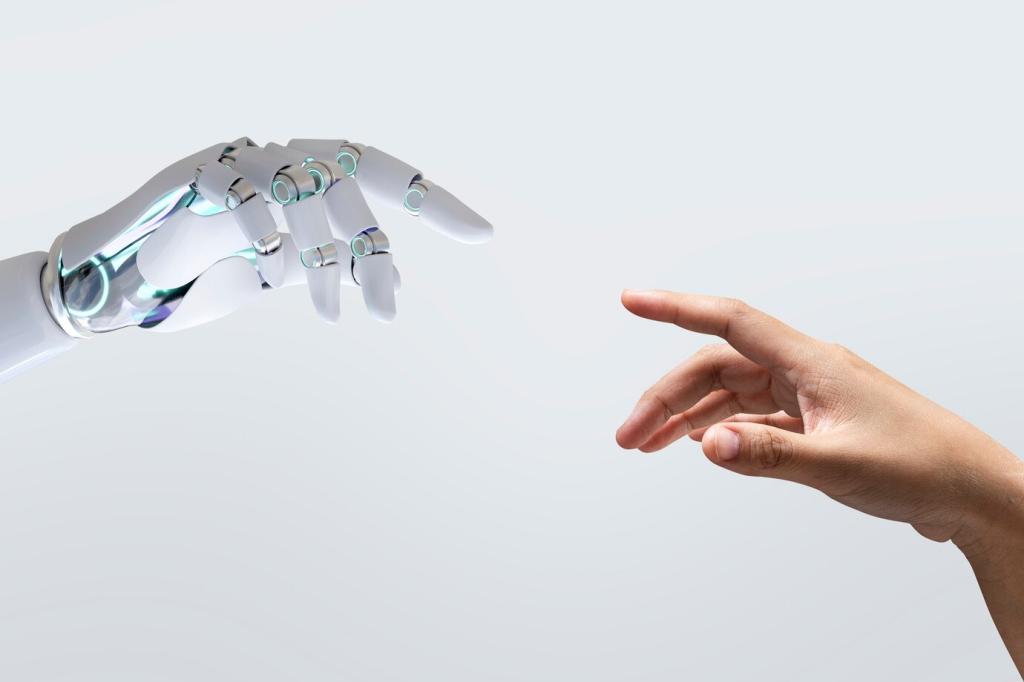
Predictive analytics is revolutionizing medical diagnosis by harnessing the power of data, machine learning, and advanced algorithms to identify patterns that might be invisible to the human eye. With an ever-increasing volume of patient information being collected, the healthcare industry is uniquely positioned to benefit from analytical tools that forecast the onset and progression of diseases. Predictive analytics empowers healthcare providers to move from reactive care—treating illnesses as they appear—to proactive intervention, where risks are identified and addressed before symptoms manifest. This shift not only enhances clinical outcomes but also optimizes resource allocation and reduces costs for healthcare systems. Ultimately, predictive analytics is driving a transformation in how physicians diagnose, treat, and manage patient health.
Data Collection in Healthcare
Machine Learning Algorithms
Model Validation and Accuracy
Clinical Applications of Predictive Analytics
Data Privacy and Security
Integration with Clinical Workflows